There appears to be some confusion, misunderstanding, and unfounded concern about state governments being asked to adopt the recent initiative from the U.S. Department of Defense regarding a dental health provider’s compact for U.S. states and territories [1]. Yet, there needs to be a realization of the significance and priority for joining the Dentist and Dental Hygienist Compact, since it directly incorporates into health care security as a strategy component. While there is a gross lack of research and information shared in this area, this article serves to offer such research, information, insight and clarification on the value and necessity of a dental compact agreement for all U.S. states and territories.
DENTAL COMPACT DESCRIPTION*
The Dentist and Dental Hygienist Compact is a contract among states that utilizes mutual recognition of licensure by privileging dentists and dental hygienists to practice in states where they do not currently hold a license. The compact privilege is equivalent to a license and grants the practitioner the full scope of practice authorized in states where such privilege is granted (FIGURE 1). Regulators in compact states will access a secure database system which holds dentists’ and dental hygienists’ continuously updated licensure information, including any disciplinary actions or investigations. It is from this database that privileges may be granted or denied.
The compact does not control or mandate the state’s licensure requirements or scope of practice. Any state belonging to the compact agrees to accept practitioners from other participating states as long as compact requirements are met. To be eligible for a compact privilege a licensee candidate must have:
- An unencumbered license in a state that has joined the compact.
- Graduated from a dental or dental hygiene education program accredited by the Commission on Dental Accreditation (CODA).
- Passed the National Board Examination.
- Completed a clinical assessment for licensure.
- Passed an FBI background check.
- Passed any jurisprudence requirements established by the participating state they wish to practice in.
- Pay all required fees.
RELEVANCE OF THE DENTAL COMPACT TO NATIONAL HEALTH CARE SECURITY
During a disaster, medical care is provided to U.S. Citizens in need by the Federal Emergency Management Agency (FEMA). FEMA then activates the National Disaster Medical System (NDMS), which in turn sends the Disaster Medical Assistance Teams (DMAT) to the site of disaster. [6]
DMATs provide quality rapid-response medical care when public health and medical emergencies overwhelm state, local, tribal, or territorial resources. In the aftermath of natural and technological disasters, acts of terrorism, and during disease outbreaks, DMAT members are on location to protect health and save lives [7].
Each DMAT team consists of the following specialties: Advanced clinicians (nurse practitioners/physician assistants), physicians, medical officers, registered nurses, respiratory therapists, paramedics (EMTs), pharmacists, safety specialists, logistical specialists, information technologists, communication and administrative specialists [7]. As one examines this medical provider list, it is evident that dentistry is absent. Obviously, this is a dangerous omission that needs correction.
Sadly, injuries during disasters and in prolonged recoveries can include dental trauma and other acute oral conditions. According to the Cleveland Medical Clinic, “A dental emergency is any injury to your mouth that causes uncontrolled bleeding, severe pain or broken facial bones. Left untreated, a dental emergency can lead to even further issues, including the spread of infection, tooth mobility and even tooth loss. Prompt, timely treatment is key” [8].
It is absolutely necessary that all dental providers have access to help with DMAT efforts. Each state needs an agreement in place to ensure proper dental health of all residents during a disaster. A comprehensive health model, such as that afforded within a dental compact agreement, may not only better serve citizens in need but also protects medical teams in the field should oral injuries or acute disease patterns arise. Not acting on this oversight now will place risks on the overall health of citizens later during an emergency.
A dental compact, once established, would also become an integral part of a time-efficient and cost-effective strategy that prevents or mitigates national/regional disasters and emergencies. The Dentist and Dental Hygienist Compact as such is consistent with the U.S. Department of Health and Human Services’ National Health Security Strategy (Strategic Goal 1) [2]. Dentists, dental hygienists and other dental auxiliaries are valuable contributors to medical surge events, and can offer a wide range of dental care expertise in a mass disaster response. Regardless of a provider’s status in the dental compact as a volunteer dentist, private practitioner, employee or paid contractor, being privileged in multiple states under the compact implements mobility of care professionals from any one compact state to another member state for any desired length of time. Thus, access to care in a compact state during an emergency can be maximized in that a uniform response of several dental professionals, having been pre-qualified, privileged through the compact, and organized into an extensive base of providers, may be mobilized relatively quickly in selected states if providers elect to participate there.
Preparedness is the process of preparation to mitigate emergencies or disasters using training, planning and organization. Readiness is a condition of having the confidence and motivation to carry out the actual mitigation tasks after appropriate preparation. The dental compact provides both of these attributes to privileged professionals while building a large provider base established within uniform standards and requirements.
A dental professional, when licensed by the compact and having mobility that the compact allows, may decide without obligation to participate in this national strategy when privileged in other states. A few of the many compact benefits, examples and rationale relevant to health care security, preparedness and readiness include:
Quickly staffing a surge event for mitigation of public health emergencies.
Licensees from other compact states may electively decide to travel to and from other compact states to practice in public dental health surge events (FIGURE 2), help mitigate public health emergencies, or offer relief from provider shortages for any desired length of time. Access to potential staffing is readily available since the compact provides an immediate source of certified providers serving over a range of member states to help in a qualified emergency response.
Decompressing state licensure review boards in an emergency.
The compact decompresses dental review boards of member states since information on applicants and licensees is collected and maintained within the compact’s secure database for reference, versus dependence entirely upon an internal state database system. In an emergency or surge, when an influx of additional care professionals is necessary, valuable time, expense and effort is saved by a compact state since there is no need to modify an internal, independent, and separate administrative computer infrastructure to review applications or licensees. Furthermore, the compact, already having been established by all member states, is a redundant and central authoritative database that can be referenced in the event a state government’s computer infrastructure is incapacitated by a cyberattack, and especially concurrent to the emergency.
Providing pre-qualified professionals speeds care mobilization and reduces risks to the public during emergencies.
As implied above and despite any non-compact state’s process for efficiently licensing of out-of-state applicants (even for temporary licenses), there will be delays and a critical time loss interim to authorizing a professional’s direct care to patients. This especially impacts residents in underserved areas with acute or long-term shortages of care professionals. Also, leaving areas unattended with widespread acute and urgent needs creates multiple complications that may challenge or limit emergency management effectiveness. The compact already provides a base number of professionals with privileges in a subject state. This supplements planning for quick and effective action for mitigation and control of emergencies and/or surge events.
Compact privileges are already compatible with current dental professional training programs.
With few differences, certified dentist and dental hygienist training programs throughout the U.S.A. are largely considered to be mostly equivalent in the level, standards and scope of education for eligibility of licensure anywhere in the U.S. including within a dental compact. Thus, it is understandable that the Dentist and Dental Hygienist Compact has the official endorsement of the American Dental Association (ADA), American Dental Hygienists’ Association, American Dental Education Association (ADEA), American Student Dental Association and other authoritative oral health organizations nationwide [3].
Serving the national interest in a declared military action
It may easily be construed that in the case of a large-scale surge requirement for extensive dental prevention, treatment and stabilization of service members at military facilities and clinics, the compact can be an immediate source for mobilizing pre-qualified licensees privileged across member states to help clear dental conditions of personnel and maximize their readiness before deployment [5].
CONCLUDING INFORMATION AND COMMENTS
As of the date of this article, only 10 U.S. states have agreed to participate in the Dentist and Dental Hygienist Compact [1]. It is noteworthy that currently, there is a U.S. medical licensure compact and a nurse’s licensure compact, each with 42 members consisting of 40 U.S. states, the territory of Guam and the District of Columbia [4]. Physicians and nurses in these compacts are ready to serve within practice formats that are similar to that of the dental compact. Similarly, any state that joins the dental compact not only brings the potential improvement of health care for its residents as well as those of any other member states, that state also advances participation for national health care security, preparedness, and readiness. Finally, it is implicit from the COVID 19 pandemic that we should not wait for the next crisis to begin joining a large partnership of cooperating states to mitigate emergencies. Now is the time for all states to join this compact for the collective good of the country.
*Dental Compact Description provided by the National Center for Interstate Compacts- Council
of State Governments, Lexington, KY
REFERENCES
- Dentist and Dental Hygienist Compact www.ddhcompact.org (last accessed 8/8/24).
- U.S. Department of Health and Human Services – Administration for Strategic Preparedness and Response, National Health Security Strategy, Strategic Goal 1 https://aspr.hhs.gov/NHSS/Pages/default.aspx (last accessed 7/15/24)
- Dentist and Dental Hygienist Compact https://ddhcompact.org/letters-of-support/ (last accessed 7/15/24).
- https://www.imlcc.org/, https://www.imlcc.org/participating-states/ https://www.nursecompact.com/ (last accessed 7/15/24).
- https://media.defense.gov/2022/Oct/27/2003103845/-1/-1/1/2022-NATIONAL-DEFENSE-STRATEGY-NPR-MDR.PDF (page 18, VII-Force Planning), (last accessed 7/15/24).
- Federal Emergency Management Agency: National Disaster Medical System (NDMS): Disaster Medical Assistance Teams (DMAT) & Definitive Care. https://www.fema.gov/emergency-managers/practitioners/recovery-resilience-resource-library/national-disaster-medical (Last Accessed 7/15/24).
- U.S. Department of Health and Human Services: Disaster Medical Assistance Teams. https://aspr.hhs.gov/SNS/Pages/Disaster-Medical-Assistance-Teams.aspx (Last Accessed 7/15/24).
- Cleveland Medical Clinic: https://my.clevelandclinic.org/health/articles/11368–dental-emergencies-what-to-do (Last Accessed 7/15/24).
FIGURE 1
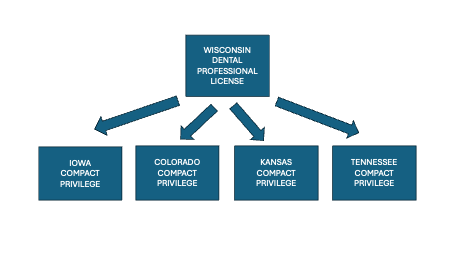
A license holder in a compact state (Wisconsin) can apply for equivalent practice privileges in any other state(s) participating in the compact. In this example, the Wisconsin license holder can obtain privileges in any number of other states that are compact members, such as Iowa, Colorado, Kansas and Tennessee.
FIGURE 2

Public dental health surge events are presently being offered at various times and locations throughout the country. These events often involve volunteer personnel providing care to the underserved with portable equipment inside large buildings as temporary field clinics. Such clinical settings would appear much like those expected in a declared emergency. Photo courtesy of Wisconsin Dental Association.
AUTHORS
Gregory S. Jacob, BS, MS, BS, DDS Glenview, IL
Karin Buchanan, PhD, RN, APN, NHDP-BC, CCRN, CEN Trauma Services Manager Ascension St. Alexius Medical Center Barrington, IL
Jamie Johnson, PhD. Professor Assistant Director of the School of Law Enforcement and Justice Administration Western Illinois University Stipes Hall 404 Macomb, IL
